Rudenko E.
Educational Institution Belarusian State Medical University
Early in XXI century,
On the one side, such a wide prevalence of D hypovitaminosis is caused by objective demographic changes: evident population aging and natural growth of geriatric pathology due to either age disorders of functional regulation of organism or life conditions of elderly persons (unbalanced nutrition, low physical activities, insufficient sun exposure), on the other hand climatic changes related mainly to people activities (more cloudy days, less insolation inhibit Vitamin D production in organism). Shift of solar zenith angle subject to terrestrial latitude, season of the year or time of the day influences significantly Vitamin D3 (Cholecalciferol) synthesis. In areas of latitudes above or under 33o the production of Cholecalciferol is least intensive or absent during the most part of winter [4].
In the Republic of Belarus over 50% of women of all age groups evidence low Vitamin D in serum regardless of seasons; the rate of D hypovitaminosis is 79% in
In recent years, genetic predisposition to DVD has been actively studied. The vitamin D receptor gene (RVD) is one of the central regulators in the endocrine system and acts as a candidate gene that determines the characteristics of human growth. It has been proven that mutations of this gene lead to rickets, osteomalacia, growth retardation, bone deformations and secondary hyperparathyroidism [1,4]. In addition, new data indicate the likely role of RVD polymorphism in the pathogenesis of bone damage and the development of secondary osteoporosis in rheumatoid arthritis and other autoimmune diseases [7,8].
Of particular interest in recent decades is the study of the role of vitamin D and its active metabolites in the functioning of the components of the immune system: lymphocytes, monocytes and dendritic cells. Studies have appeared that indicate the ability of 1,
Figure 1. Stages of Vitamin D metabolism.
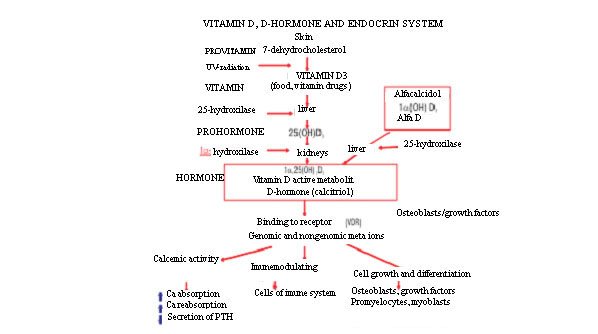
Figure 1. Vitamin D production, basic stages of its Metabolism and biological effect [13]
The term «Vitamin D» is defined as a group of chemicals used by each steroid, including the use of vitamins D2 (Ergopcalcipherol) and D3 (Cholecalciferol). Ergopcalcipherol is primarily found in plants derived from ergosterol, and cholecalciferol is a
Synthesized in skin under UV rays, Cholecalciferol binds to specific vitamin D binding protein (DBP) (transcalcipherin) and is transferred to liver. Then in endoplasmic reticulum of hepatocyte its hydroxylation occurs at the 25th carbon atom with 25 (OH) D3 (Calcidol) formation, the latter binds to
In bone tissue, Calcitriol stimulates the expression of
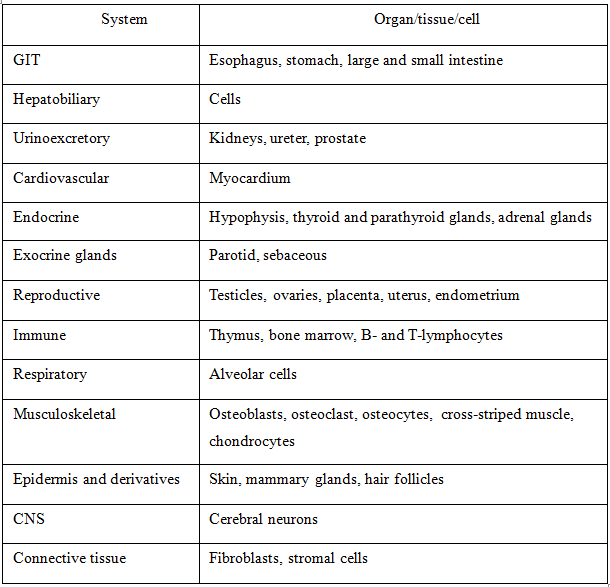
By interaction with VDR 1,25(OH)2D3 develops its genomic effect in various organs and cells presented in Table 1 1 [13].
Table 1 — Principle organs and cells with VDR
Vitamin D deficiency diagnostics
Currently, the clinical department of laboratory diagnostics is equipped with available standardized methods for determining its status in organism. DVD is detected using reagent kits to determine the level of total 25 (OH) D (includes 25 (OH) D2 and 25 (OH) D3) in blood serum using modern methods of mass spectrometry, competitive protein binding, high performance liquid chromatography, and
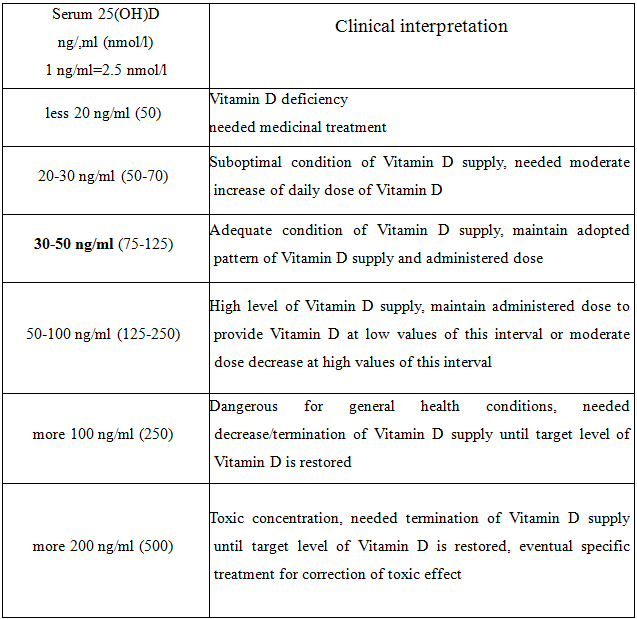
The serum concentration of total
To clarify the bone pathology caused by vitamin D deficiency, it is necessary to assess the levels of PTH, calcium, phosphorus, ALP, magnesium, β-
Reference data of 25(OH)D level n and their interpretation are presented in Table 2. This concept of clinical interpretation of Calcidol level was developed by a large group of scientists within 200/2013 under the direction of Prof. P.Pludovsky and published in Practical recommendations on Vitamin D supply and treatment of its deficiency in the countries of Central Europe [15].
Table 2 — Reference parameters of 25(ОН)D in blood serum and their clinical interpretation
Indications to determine 25(ОН) D in blood serum:
1. Elderly persons staying long indoors;
2. Differential diagnostics of skeleton metabolic diseases (rachitis, osteomalacia, osteoporosis, etc.);
3. Detection of autoimmune and oncological diseases;
4. Apparent deficiency or extra body weigh/obesity;
5. Celiaс disease, malabsorption;
6. Before administration of osteoporosis therapy;
7. Menopause in women, hypogonadism in men;
8. Evaluation of dynamics in long intake of high doses of Vitamin D;
9. Emigrants from southern territories.
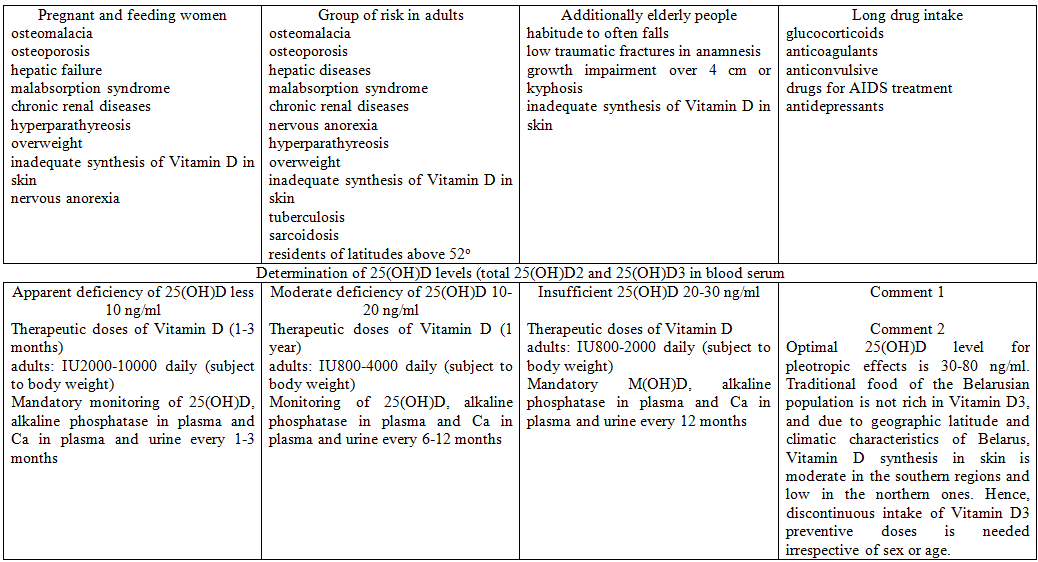
In 2013, the Ministry of Health of the Republic of Belarus approved the instructions for use «Methods for the diagnosis, prevention and differentiated treatment of vitamin D deficiency» (registration number 033–031313 from 06/14/2013) [16]. An appendix to this instruction is an algorithm for the diagnosis and prevention of DVD, which can be used to identify risk groups, determine indications for a study of the plasma level of 25 (OH) D and to determine the required dose of Cholecalciferol (Fig. 2).
Algorithm of diagnostics and prophylaxis of Vitamin D deficiency in the Republic of Belarus Vitamin deficiency group of risk
Correction methods of Vitamin D deficiency:
1. Healthy foods;
2. Food fortification with Cholecalciferol;
3. Sufficient natural sun exposure (main source);
4. UV tubes;
5. Ergocalciferol (D2) intake;
6. Cholecalciferol (D3) drugs’ intake;
7. Active metabolites of Vitamin D;
8. Parenteral introduction of Vitamin
Recommendations for diet
These foods have relatively high levels of vitamin D: fatty varieties of marine fish. scomber, salmon, tuna, mackarel and herring are sources of vitamins D. The liver of cod and halibut, caviar, seafood, oil sprats, beef and pork liver, cheese, egg yolks, cheese, and butter are also rich in vitamin D. The highest content of Vitamin D in fish oil, 100 grams of which contains 250 micrograms of vitamin. Prepackaged gelatin capsules contain IU500 of vitamin A and IU50 of vitamin D. It is worth noting that the composition of fish oil also includes Vitamin A (30,000 g per 100 grams), which overdose is characterized by headache, weakness, dry skin, joint pain, cracked lips, rare hard hair, dry rough skin. It should be remembered that high doses of vitamin A are teratogenic. Potato, parsley, nuts, seeds, mushrooms, oatmeal, and products such as urtica, horsetail, dandelion greens, and lucerne should be noted among plant foods containing vitamin D.
Publications provide tables on the content of vitamin D in foods. However, in general, in the daily diet with the nutrition traditional for Belarusians, its content is no more than
Scientists estimate that only wheat flour enrichment reduced D hypovitaminosis in the population of country D by 25% [17].
The main source of vitamin D for most people is its formation when exposed to sunlight on the skin, usually within 1000–1500 hours in spring, summer and autumn. Vitamin D formed in the skin can remain in blood at least twice as long as supplied with food. When an adult in a bathing suit is exposed to one minimal erythema dose of ultraviolet radiation (a slight pinking of the skin 24 hours after exposure), the amount of vitamin D produced is equivalent to ingestion of
The synthesis of Cholecalciferol in human skin can be influenced by many factors, the most significant of which are the use of sun protective aids, skin pigmentation, the presence of scars after burns, psoriasis, decrease in the content of
Pharmacological correction of D hypovitaminosis
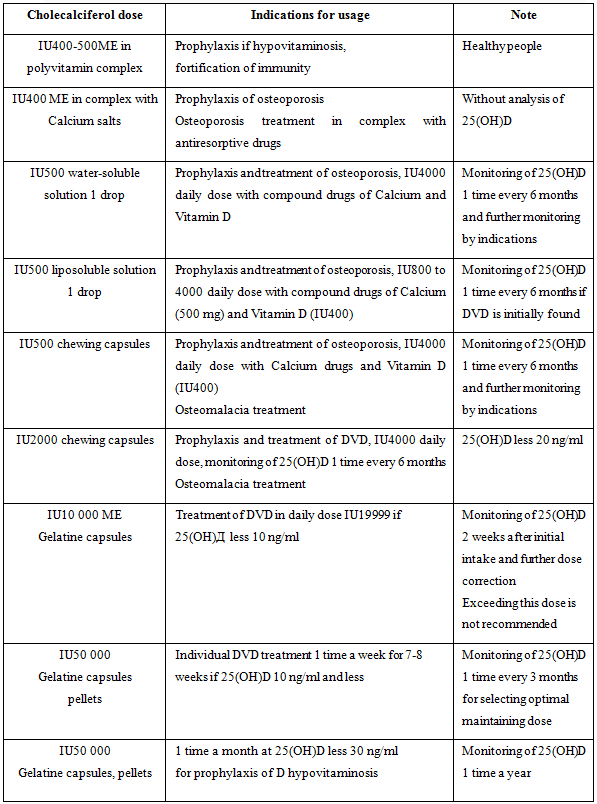
Cholecalciferol and its active metabolites are available in market as solutions, capsules, pellets IU200 to IU50000. In clinical practice doctors of various specialization DVD monotherapy subject to 25(OH)D level adopts either high individual doses or lower doses for prophylaxis and treatment (
Table 3, compiled on the basis of generalization of the data obtained during the study of international recommendations for the diagnosis and correction of D hypovitaminosis, gives indications for administration of vitamin D3 in various doses, depending on initial 25 (OH) D and the incidence of laboratory tests to monitor its status in order to clarification of the need for correction of ongoing therapy and the exclusion of a possible overdose of Cholecalciferol [14,18,19].
Table 3. Indications for usage of prophylactic and therapeutic doses of Vitamin D3
According to practical recommendations proposed by the US Institute of Medicine in 2011, a differentiated approach to prescribing daily doses of Cholecalciferol from IU400 IU10000 can be recommended for the prevention of DVD [18]. Some aspects of these recommendations are presented below:
1. For healthy population aged 18–50 years, with the aim of preventing DVD, it is recommended to receive at least
2. Persons over 50 years of age for the prevention of DVD need at least
3. In recent
4. Scientific studies in people over 65 to evaluate the effect of IU800 of vitamin D per day on muscle strength, impaired coordination of movements and the frequency of falls revealed the following results: muscle strength increased by 4–7%, coordination of movements improved by 28%, and incidence of falls decreased by 35–72% based on reports from various sources.
5. Pregnant and feeding women for DVD prophylaxis need at least
5. For people with overweight or malabsorption Vitamin D3 daily dose can be increased to IU4000 and over.
Table 4 summarizes various doses of Cholecalciferol drugs registered by Minskintercaps U.
Table 4 — Cholecalciferol drugs registered in MH Belarus by pharmaceutical enterprise Minskintercaps U.V.
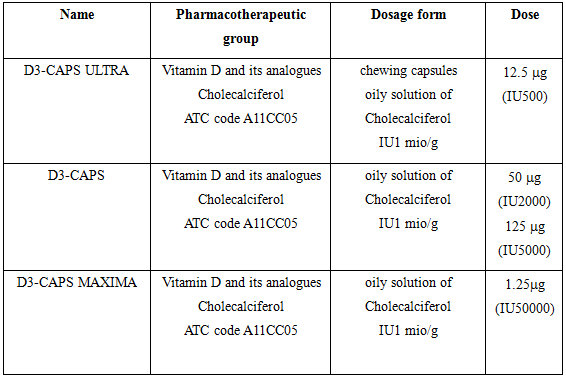
Note. 1 mg=IU40
Signs of Vitamin В overdose and intoxication are rare and associated mainly with high doses for a long period. Clinical symptoms in this case are anorexia, nausea, polyuria, constipation, asthenia, weight loss, headache, depression, thirst, muscular rigidity, soft tissue calcification, nephrocalcinosis, and hypertension.
Laboratory signs confirming an overdose of vitamin D are hypercalcemia, hypercalciuria (urine Ca ratio (mmol / L) / urine creatinine (mmol / L) more than 0.57), an increase in 25 (OH) D level above 100 ng / ml. Hypercalcemic crisis, developing with an increase in blood calcium levels to 4 mmol / l, can lead to death as a result of inhibition of nervous activity and coma.
Contraindications of vitamin D3 drugs in adults are: hypercalcemia, hypercalciuria, nephrocalcinosis, nephrolithiasis, hypervitaminosis, a tendency to allergic reactions to components of the composition of the drug. Vitamin D preparations are not prescribed for granulematosis, sarcoidosis, bone metastases, Williams syndrome due to the increased risk of hypercalcemia and hypercalciuria [13,14,20].
Conclusion. When prescribing calcium and vitamin D preparations, the attending physician should make every effort to achieve an adequate adherence to treatment and to obtain the best result in relation to primary and secondary prevention of osteoporotic fractures. At the same time, regular laboratory monitoring of
REFERENCES
1. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008 Apr;87(4):
2. Cashman KD, Dowling KG, Skrabakova Z,
3. P. Pludowski,
4. Spiro A, Buttriss JL. Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39:322–50. http://www. ncbi.nlm.nih.gov/pmc/articles/PMC4288313/
5. Vitamin D status in residents of Belarus: analysis of the
6. Provision rating of Vitamin D in post menopausal women in Belarus. E.
7. Pludowski P, Holick MF, Pilz S, Wagner CL, Hollis BW, Grant WB, Shoenfeld Y, Lerchbaum E, Llewellyn DJ, Kienreich K, Soni M. Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and
8. Mukhtar M, Sheikh N, Suqaina SK, et al. Vitamin D Receptor Gene Polymorphism: An Important Predictor of Arthritis Development. Biomed Res Int. 2019;2019:8326246. Published 2019 Mar 18. doi:10.1155/2019/8326246
9. Eisman JA, Bouillon R. Vitamin D: direct effects of vitamin D metabolites on bone: lessons from genetically modified mice. Bonekey Rep. 2014;3:499. Published 2014 Feb 5. doi:10.1038/bonekey.2013.233
10. Aikaterini I. Trochoutsou, Vaia Kloukina, Konstantinos Samitas and Georgina Xanthou, «
11. F. Colotta, B. Jansson, F. Bonelli, Modulation of inflammatory and immune responses by vitamin D, J. Autoimmun. 85 (2017) 78–97. doi:10.1016/j.jaut.2017.07.007.
12. Erin Yamamotoa Trine N.Jørgensen. Immunological effects of vitamin D and their relations to autoimmunity. Journal of Autoimmunity Volume 100, June 2019, pp.7–16
13. Shvarts
14. Charoenngam N et al., Vitamin D for skeletal and
15. Vitamin D supplementation guidelines / P.Pludowski, [et al.] // J. Steroid. Biochem. Mol. Biol. — 2018 — Vol. 175,(Jan). — P. 125–135.
16. Diagnostic technique, prophylaxis and differential treatment of Vitamin D deficiency. Instruction for usage Registration #033–0313: approved
17. M. Aguiar, L. Andronis, M. Pallan, W. Högler, E. Frew. The economic case for prevention of population vitamin D deficiency: a modelling study using data from England and Wales European Journal of Clinical Nutrition, March 2019 https://doi.org/10.1038/s41430-
18. Holick MF, Binkley NC,
19. Vitamin D deficiency in adults: treatment and prophylaxis. Russian Association of endocrinologists, 2015 // http://specialist.endocrincentr.ru. — Access date: 15/05/2016
20. Instruction for usage of D3 caps is available on site http://from