 Belarusian State Medical University, Minsk, Belarus
Belarusian State Medical University, Minsk, BelarusSummary. A review of the literature on the prevalence and causes of hypovitaminosis D in the world and the Republic of Belarus is given. Risk factors that affect the level of vitamin D in the human body are identified. The stages of vitamin D metabolism and its main biological effects are described. Modern methods of laboratory diagnosis of the status of vitamin D in blood serum are presented. The concept of the clinical interpretation of reference data of levels 25(OH)D is given. Schemes of individual correction of deficiency and hypovitaminosis D in risk groups according to modern international recommendations are proposed.
Keywords: vitamin D, hypovitaminosis D, deficit D, 25(OH)D, cholecalciferol.
At the beginning of XXI century the problem of hypovitaminosis D acquired not only medical but also medical-social value. According to statistics more than 1 billion people in the world are vitamin D deficient. Vitamin D status studies, made in Europe, by measuring concentration of total 25(OH)D in blood demonstrated that only 13% in the surveyed population have its suboptimal level [13,18,17].
On the one hand, the reasons of such high prevalence of hypovitaminosis D are objective demographic changes: noticeable aging of the population and regular growth of geriatric pathology due to age-related disorders of the regulation of organism functions and living conditions of older people (unbalanced nutrition, low level of physical activity, insufficient sun exposure); on the other hand – climate changes which are largely related with human activity (the increase in the number of cloudy days and the decrease in insolation reduce vitamin D formation in the organism). The changing of the sun zenith angle depending on geographical latitude, season or time of the day significantly affects on synthesis of vitamin D3 (cholecalciferol). In areas, located at latitudes above and below 33°, cholecalciferol production in skin occurs at very low intensity or it is absent during most of the winter.
In Belarus more than 50% of women of all age groups have a low level of vitamin D in blood serum not depending of time of a year, in women older 60 in autumn-winter season the frequency of hypovitaminosis D is 79%, in spring-summer season – 75%. In old men in autumn-winter season the frequency of hypovitaminosis D is 73%, in spring-summer season – 57% [18, 4].
In recent years genetic predisposition to vitamin D deficiency is being actively studied. Vitamin D Receptor Gene (VDR) is one of the central regulators in endocrine system and acts as a candidate-gene determining the characteristics of human growth. It is proven that mutations of this gene lead to the development of rickets, osteomalacia, stunted growth, bone deformities and secondary hyperparathyroidism [13, 19]. Besides, new data indicate the likely role of VDR polymorphism in the pathogenesis of bone damage and the development of secondary osteoporosis in rheumatoid arthritis and other autoimmune diseases [14,15].
Of particular interest in recent decades are studies of vitamin D role and its active metabolites in maintenance of functioning of the components of the immune system: lymphocytes, monocytes and dendritic cells. Studies appeared testifying of ability of 1,25-dihydroxyvitamin D3 to induce fusion processes and differentiation of macrophages, to reduce the production of inflammatory mediators in autoimmune diseases, to regulate cellular response to oxidative stress [15,9]. It was found more than 30 positive effects of vitamin D on the immune system, that allows to initiate further studies of the possibilities of its application in the treatment of autoimmune diseases [7,10,20].
The term “vitamin D” combines the group of similar in chemical structure secosteroids, where the greatest application belongs to vitamin D2 (ergocalciferol) and D3 (cholecalciferol). Ergocalciferol is mainly formed in plants from ergosterol, cholecalciferol is formed from 7-dehydrocholesterol in the human or animal organism under the influence of sun lights.
Picture 1 shows the main stages of formation, metabolism of vitamin D and its main biological effects [5].
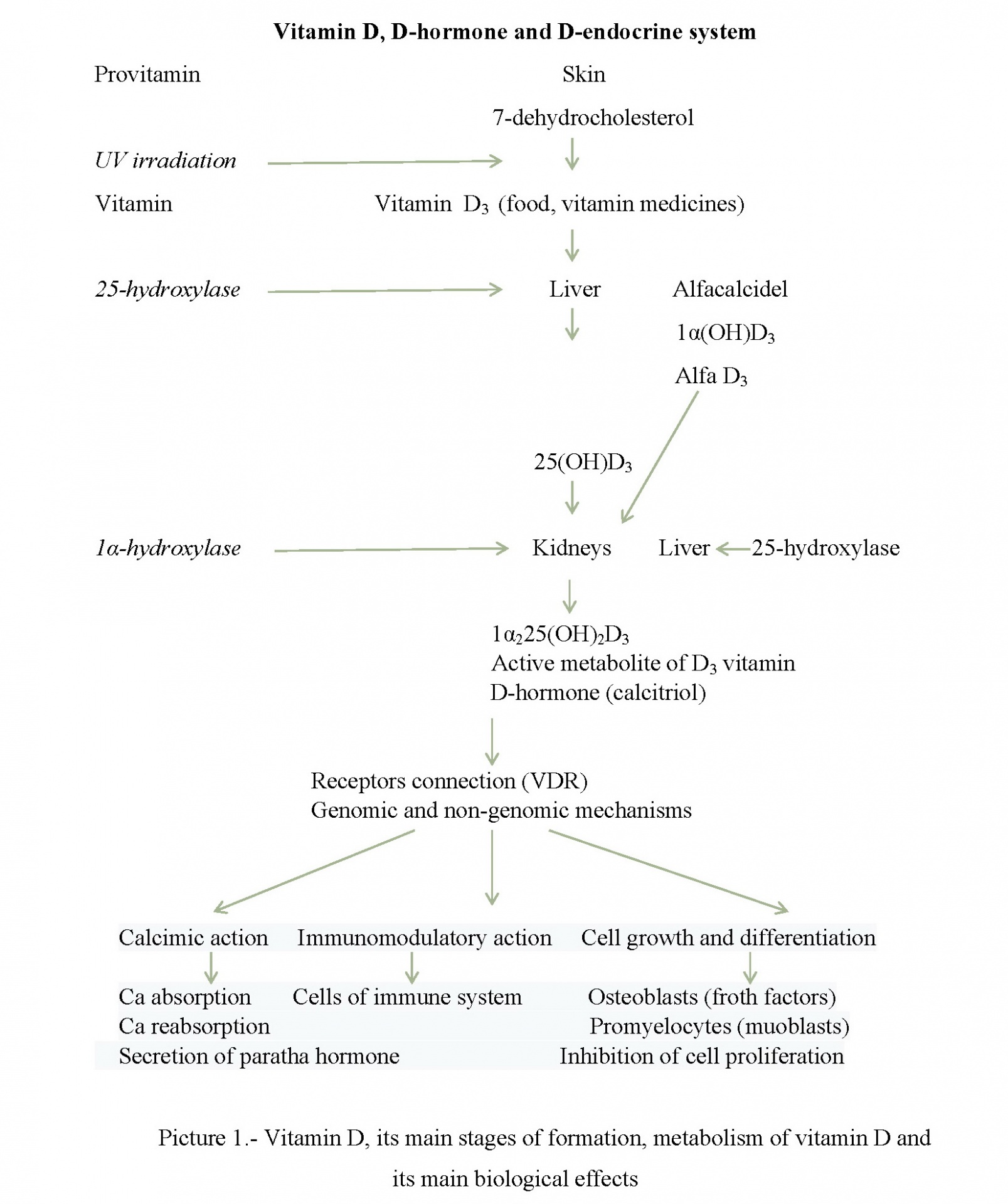
Synthesized in skin under the influence of ultraviolet lights cholecalciferol binds to specific vitamin D binding protein (transcalciferin) and is transported into liver. Then in the endoplasmic reticulum of hepatocytes its hydroxylation at the 25th carbon atom to form 25 (OH) D3 (calcidol) occurs which binds to alpha globulin and circulates in blood, without affecting calcium metabolism. The next stage of hydroxylation of 25 (ОН)D3 occurs under the influence of the enzyme 1-alpha-hydroxylase occurs in proximal renal tubule cell mitochondria. As a result active metabolite of vitamin D – 1,25(ОН)2DЗ (calcitriol) and 24,25(ОН)2D3 - is synthesized. The first one is called D-hormone recently since this form of vitamin D takes part in regulation of calcium-phosphorus metabolism and also carries out various biological effects by interacting with specific nuclear receptors for vitamin D (VDR), the second one controls the concentration of parathyroid hormone (PTH) [15, 5].
The so-called skeletal effects of calcitriol play a significant role in regulation of metabolic processes occurring in bone tissue. Under the influence of D-hormone intestinal absorption of calcium and its reabsorption in the kidneys are accelerated. Calcitriol enhances intestinal absorption of calcium in the small intestine by stimulating the synthesis of calcium-binding protein in enterocytes – calmodulin. In turn, calmodulin transports calcium ions through the intestinal wall and the system of lymphatic vessels into the circulatory vascular bed. A sufficient plasma level of calcitriol enhances the effectiveness of intestinal absorption of ionized calcium in 2-3 times and phosphorus - up to 80%. In such way processes of calcium reabsorption in the renal tubules are carried out.
In bone tissue calcitriol enhances the expression of the ligand of the receptor activator of nuclear factor kV (RANKL), accelerates the proliferation of osteoblasts, the synthesis of osteocalcin, collagen and glycosaminoglycans. 1,25(OH)2D – a powerful stimulator of osteoclastogenesis in vitro, with the introduction of high doses 1.25 (OH) 2D binds to RVD on osteoblasts and increases expression and release of RANKL [10, 9].
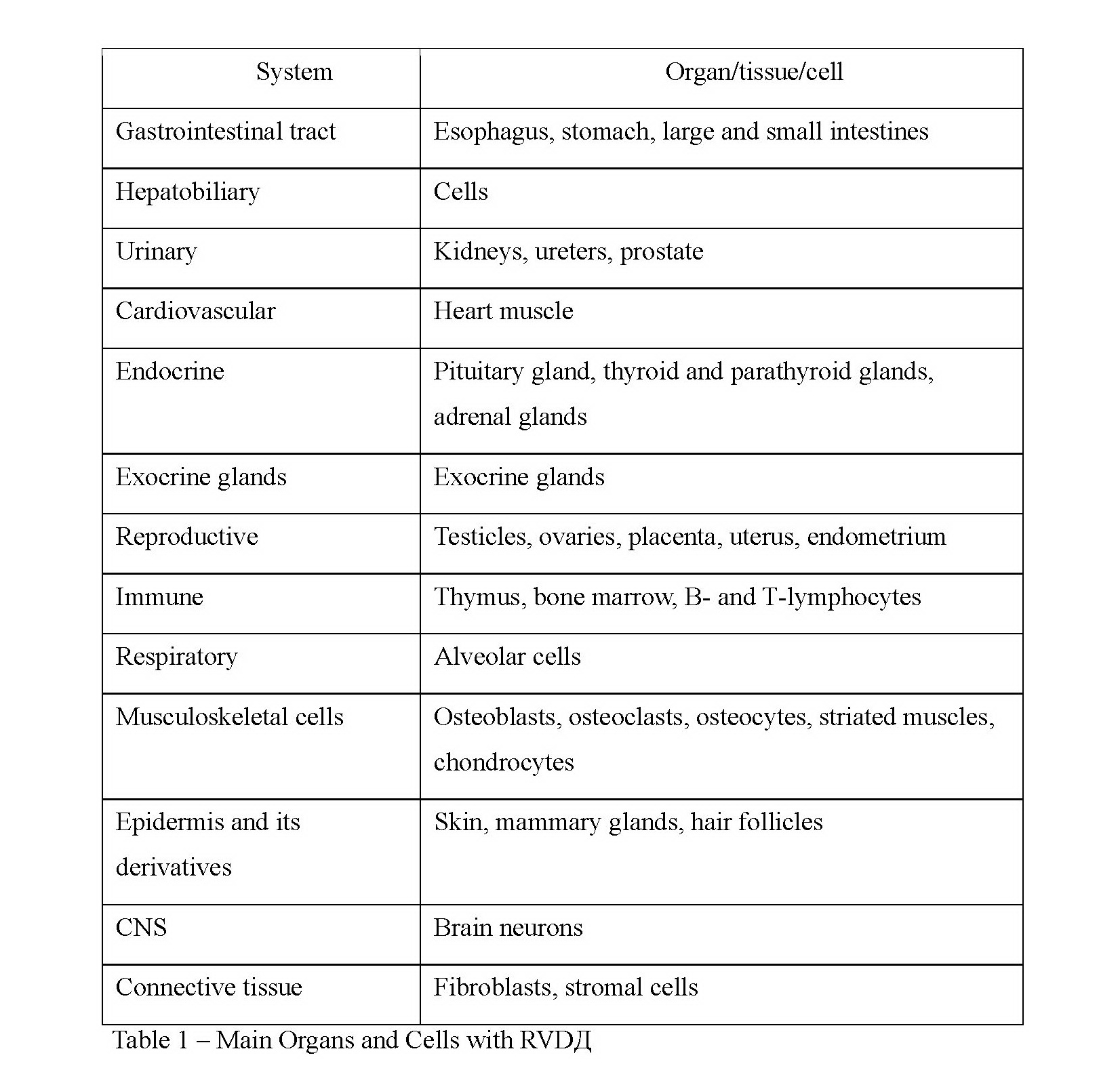
Through interaction with RVD 1,25(OH)2D3 shows its genomic effects in different organs and cells, presented in the table 1 [5].
Diagnostics of vitamin D deficiency.
Currently clinical departments of laboratory diagnostics are equipped with accessible standardized methods of determination of its status in the organism. In laboratory tests verification of the reliability of the method used in clinical practice for the determination of 25 (OH) D (by international abbreviation) is necessary regarding international standards, using the same method in the same laboratory. DVD is detected using reagent kits for the determination of total 25 (OH) D concentrations, including 25(OH)D2 and 25(OH)D3 in blood serum. In clinical practice today modern methods of mass-spectrometry, protein competitive binding, high performance liquid chromatography, radioimmune, enzyme immunoassay or immuno-chemiluminescent analysis are used. To assess vitamin D status while taking medicines of cholecalciferol it is recommended to take blood not less than in 3 days after the last dose. The determination of the concentration of total 25-hydroxyvitamin D, circulating in blood, is the best method nowadays for evaluation and monitoring of vitamin D status in clinical practice since it has a long half-life – about 15-16 days [13]. Serum concentration of total 25-hydroxyvitamin D depending on measurement method is expressed in nanograms per milliliter (ng/ml) or in nanomoles per liter (nmol / l). To compare results it is important to take into consideration that 1 ng / m equals 2.5 nmol / l. Levels of 25 (OH) D are variable and are heavily dependent on diagnostic methods, geographic position of a country, technical errors, human factor. To clarify the pathology of bone tissue caused by vitamin D deficiency it is necessary to evaluate PTH, calcium, phosphorus, OSPF, magnesium levels, bone resorption marker- type I collagen C-terminal telopeptide (βeta-Cross Laps ), bone matrix formation markers P1NP (type 1 procollagen N-terminal propeptide, Total P1NP) or osteocalcin in blood serum, morning urine calcium / creatinine ratio. At level 25 (OH) D less than 10 ng / ml in-depth examination of the patient is necessary to exclude osteomalacia (iliac wing biopsy), hereditary connective tissue diseases (genetic testing), the determination of 1,25(ОН)2D levels in case of chronic kidney disease. To exclude intestinal malabsorption it is important to identify markers of celiac disease and other chronic inflammatory diseases of the gastrointestinal tract [19, 5, 9].
Reference data of levels 25 (OH) D and their interpretation are presented in table 2. This concept of clinical interpretation of calcidol concentrations was developed by a large group of scientists from 2011 to 2013 under the guidance of the professor P/ Plydovsky and was published in “Practical Guidelines of vitamin D intake and treatment of its deficiency in countries of Central Europe” [16].
Indications for determination of 25 (OH) D in blood serum:
1. Elderly people living long indoors;
2. For the differential diagnosis of metabolic diseases of the skeleton (rickets, osteomalacia, osteodystrophy, osteoporosis and etc.);
3. Identification of autoimmune and oncological diseases;
4. Severe deficiency or overweight / obesity;
5. Celiac disease, malabsorption;
6. Before prescribing drugs for the treatment of osteoporosis;
7. Menopause in women, hypogonadism in men;
8. Dynamics assessment of taking high doses of vitamin D;
9. Pregnancy and lactation;
10. Overweight;
11. The presence of other risk factors for DVD.
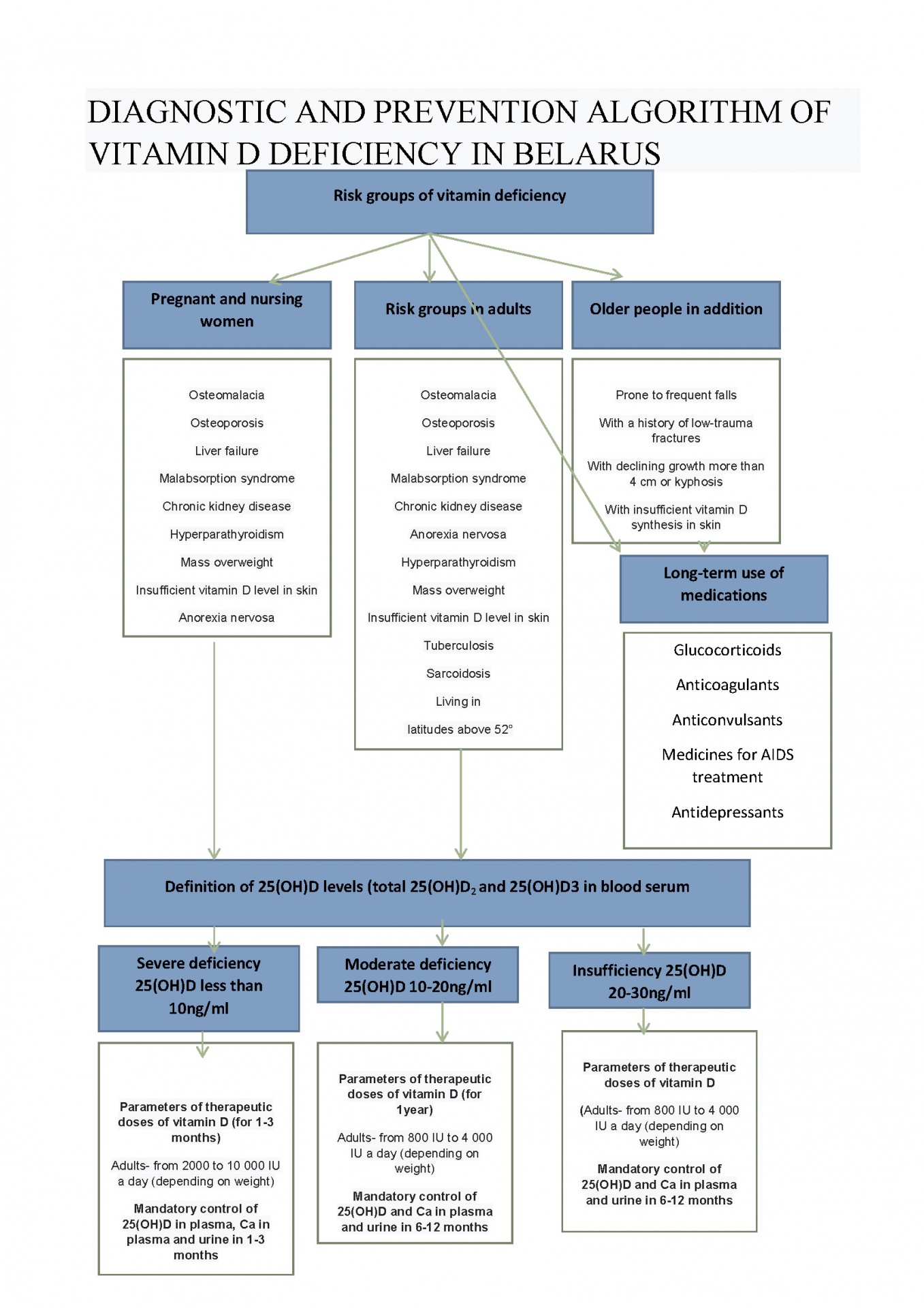
In 2013 in Health Ministry of the Republic of Belarus the instruction for use “Methods of Diagnostics, Prevention and Differentiated Treatment of Vitamin D Deficiency” was approved (registration № 033-031313 from 14.06.2013) [3]. Appendix to this instruction is an algorithm of diagnostics and prevention of DVD which can be used for identification of risk groups, determination of indications for the study of plasma levels 25(ОН) D and also for determination of necessary dose of cholecalciferol (figure 2)
Ways to correct vitamin D deficiency:
1. Food intake;
2. Fortification of food with cholecalciferol;
3. Sufficient natural sunlight;
4. Application of ultraviolet lamps;
5. Ergocalciferol intake (D2);
6. Intake of medicine forms of cholecalciferol (D3);
7. The use of active metabolites of vitamin D;
8. Parenteral administration of vitamin D.
Dietary guidelines.
Using foods of plant and animal origin a man gets not more than 100-200 ME a day. Mackerel, salmon, tuna, mackerel and herring are sources of vitamin D. Cod and halibut liver, caviar, seafood, sprats in oil, beef and pork liver, raw egg yolks, cheese, butter are also rich in vitamin D. The highest vitamin D content is in fish oil, 100 g of fish oil contain 250 mcg of vitamin. Among foods of plant origin rich in vitamin D it should be noted potatoes, parsley, nuts, seeds, mushrooms, oatmeal and such foods like nettle, horsetail, dandelion and alfalfa.
In many countries, some of the most commonly consumed foods are fortified: flour, bread, milk, juice, yogurt, vegetable oils and etc. In Great Britain the researches were held, on an economic assessment, the enrichment of wheat flour with vitamin D supplements. As a result a strong economic argument for the enrichment of wheat flour with vitamin D was approved (9.5 pounds sterling for QALY). Scientists calculated that the enrichment of wheat flour led to decrease in hypovitaminosis D in the population of country by 25% [6].
The role of sunlight.
The main source of vitamin D for a man is its emergence exposing to the skin of sunlight especially in spring and summer when there are many sunshine hours. Vitamin D, formed in the skin, can remain in the blood at least twice as much as that supplied with food. When an adult, wearing a swimming suit, receives an unimodal minimum erythema dose of ultraviolet radiation (slight pinking of the skin 24 hours after exposure) the amount of vitamin D produced is equivalent to an oral intake of 10,000-25,000 IU. Many factors can influence on the processes of cholecalciferol synthesis in human skin, the most significant ones: sunscreen use, skin pigmentation, the presence of scars after burns, psoriasis, decrease in the content of 7-dehydrocholesterol in the skin in the elderly, tome of the year, geographic position, daylight hours
Pharmacological correction of hypovitaminosis D
Cholecalciferol and its active metabolites enter the pharmacy network in the form of solutions, capsules, tablets in the doses from 200 IU to 50 000 IU. In the clinical practice of doctors of various specialties as monotherapies of DVD depending on the initial concentration of 25 (OH) D both high doses according to individual correction schemes and lower preventive and curative doses ( from 500 to 2000 IU) which do not need laboratory monitoring of vitamin D status including in combination with calcium medicines can be used.
In table 3, compiled on the basis of data compilation obtained in the study of international recommendations of diagnostics and correction of hypovitaminosis D, there are indications for vitamin D3 prescribing in various doses depending on the initial concentration of 25 (OH) D and frequency of the laboratory control for monitoring its status in order to clarify the need for correction of therapy and exclusions of a possible overdose of cholecalciferol [9,12,1].
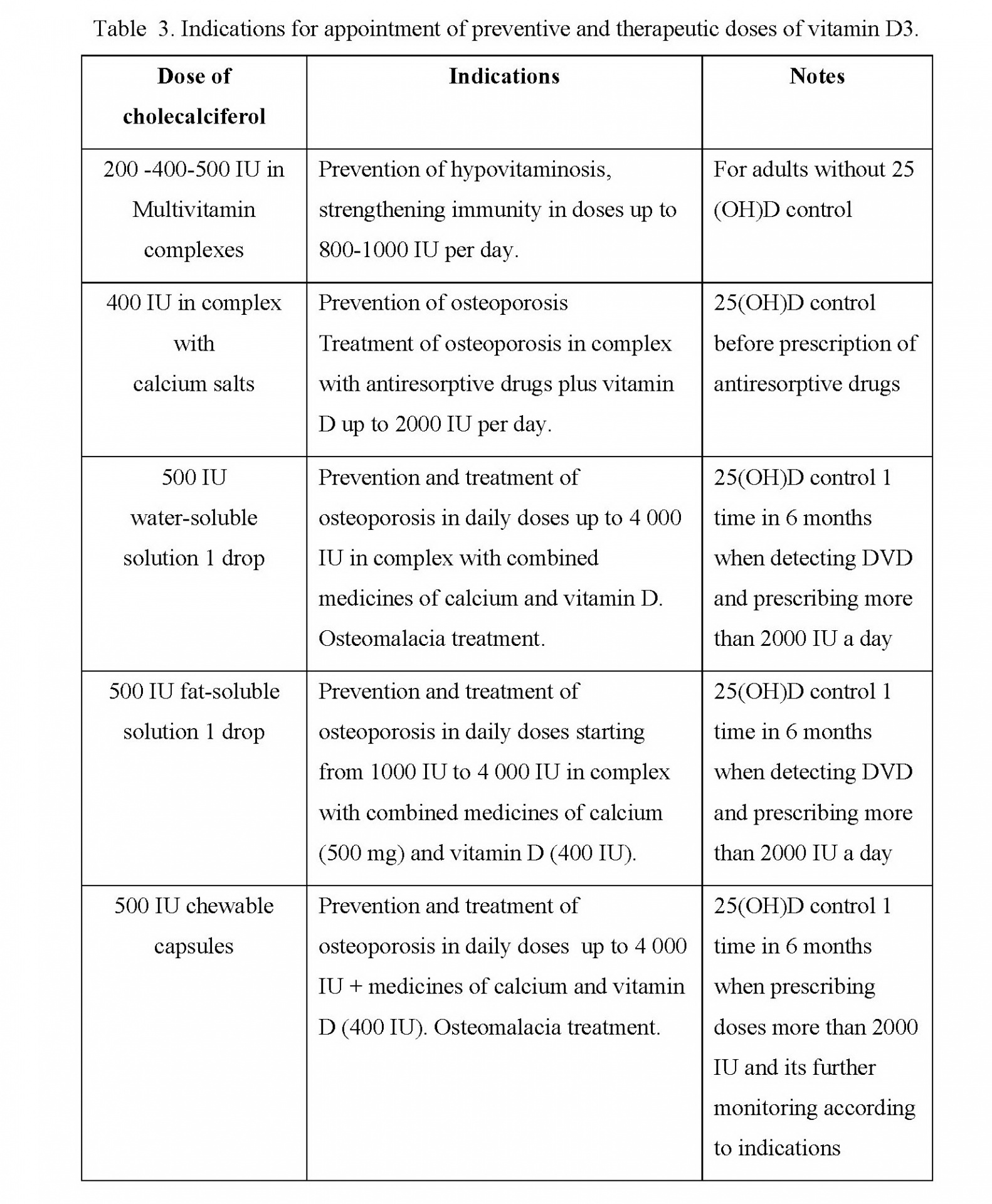
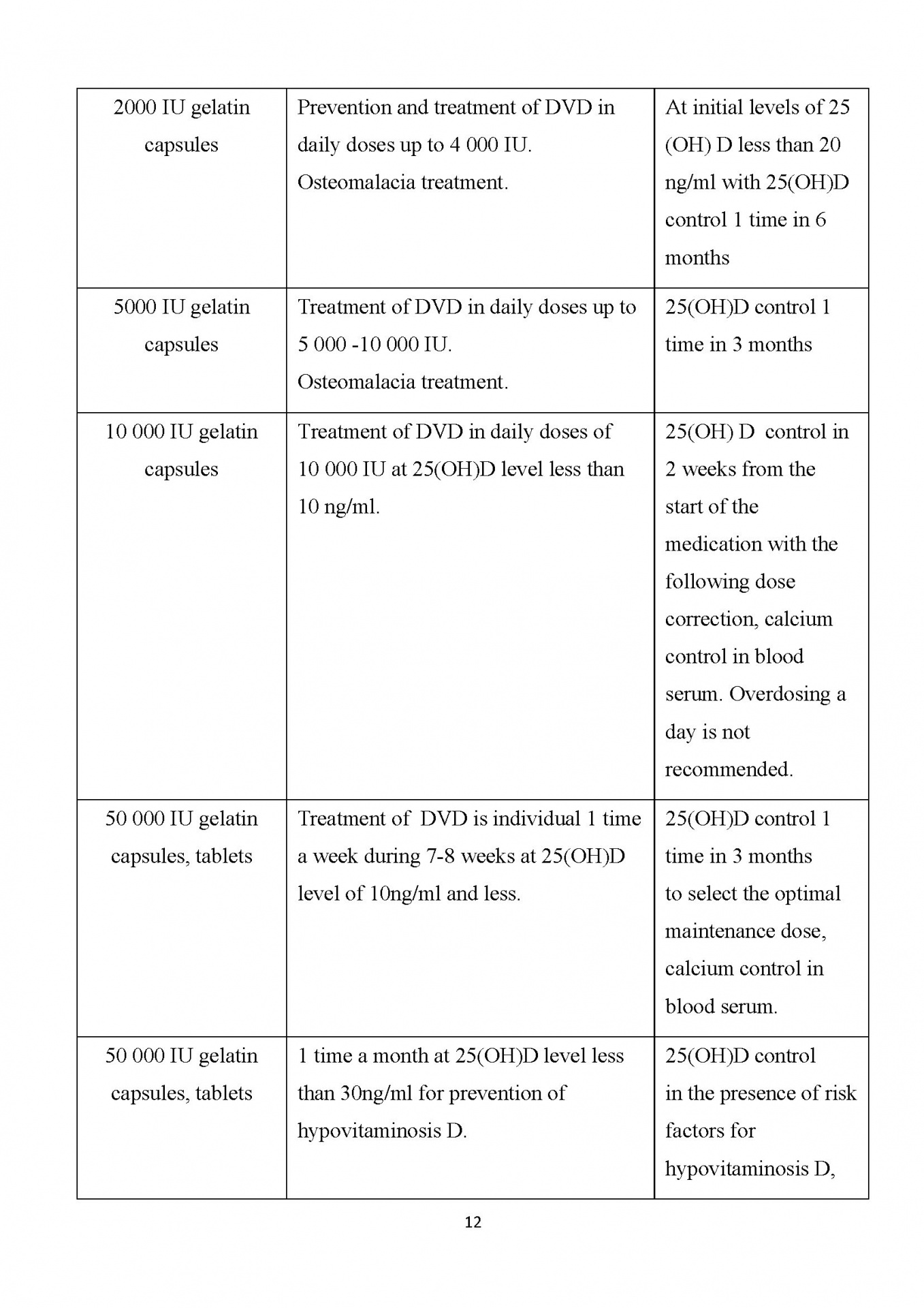
Note: upon reaching the target level of 25 (OH) D 30-40 ng / ml while taking high doses of vitamin D it is possible to go to the maintenance dose 1500-2000 IU a day.
According to practical recommendations proposed by The Institute of Medicine of the USA in 2011, differentiated approach to the appointment of daily doses of cholecalciferol from 400 IU to 10 000 IU can be recommended for prevention od DVD [12]. Some aspects of these recommendations are given below:
1. For a healthy population aged 18-50 years with the aim of prevention of DVD it is recommended to get not less than 600-800 IU of vitamin D a day to achieve suboptimal levels of 25 (OH) D greater than 20 ng / ml. To maintain a concentration of 25 (OH) D greater than 30 ng / ml it is necessary to intake 1500-2000 IU of cholecalciferol a day;
2. People older 50 years for prevention of DVD it is necessary to intake not less than 800-1000 IU of vitamin D a day;
3. In recent meta-analyzes based on double blind RCT it was demonstrated that in population of older men and women an additional intake of vitamin D in the dose of 800-1000 IU reduced any non-vertebral fractures, hip fractures and fallings by
4. Scientific researches in people older 65 years studying the effect of 800 IU of vitamin D per day on muscle strength, impaired coordination of movements and frequency of fallings produced the following results: muscle strength increased by 4-7%; movement coordination improved by 28% and frequency of fallings reduced by 35-72% according to data from different sources.
5. For prevention of DVD in pregnant and nursing women it is necessary to intake 800-1200 IU of vitamin D a day. In the presence of risk factors for DVD it is necessary to estimate the initial level of 25(OH)D depending on its levels and to choose the dose from 1500-4000 IU a day with the following control of 25(ОН)D dynamics 1 time in 3-6 months.
6. People with overweight or malabsorption daily doses of vitamin D3 can be increased up to 4000 and more a day.
In table 4 there is characteristics of medicines of cholecalciferol in different dosage forms registered by Ministry of Health of the Republic of Belarus which allows to prescribe an individual treatment regimen for DVD depending on concrete clinical situation [20].
Table 4 – Medicines of cholecalciferol registered by Minskintercaps in Ministry of Health of the Republic of Belarus
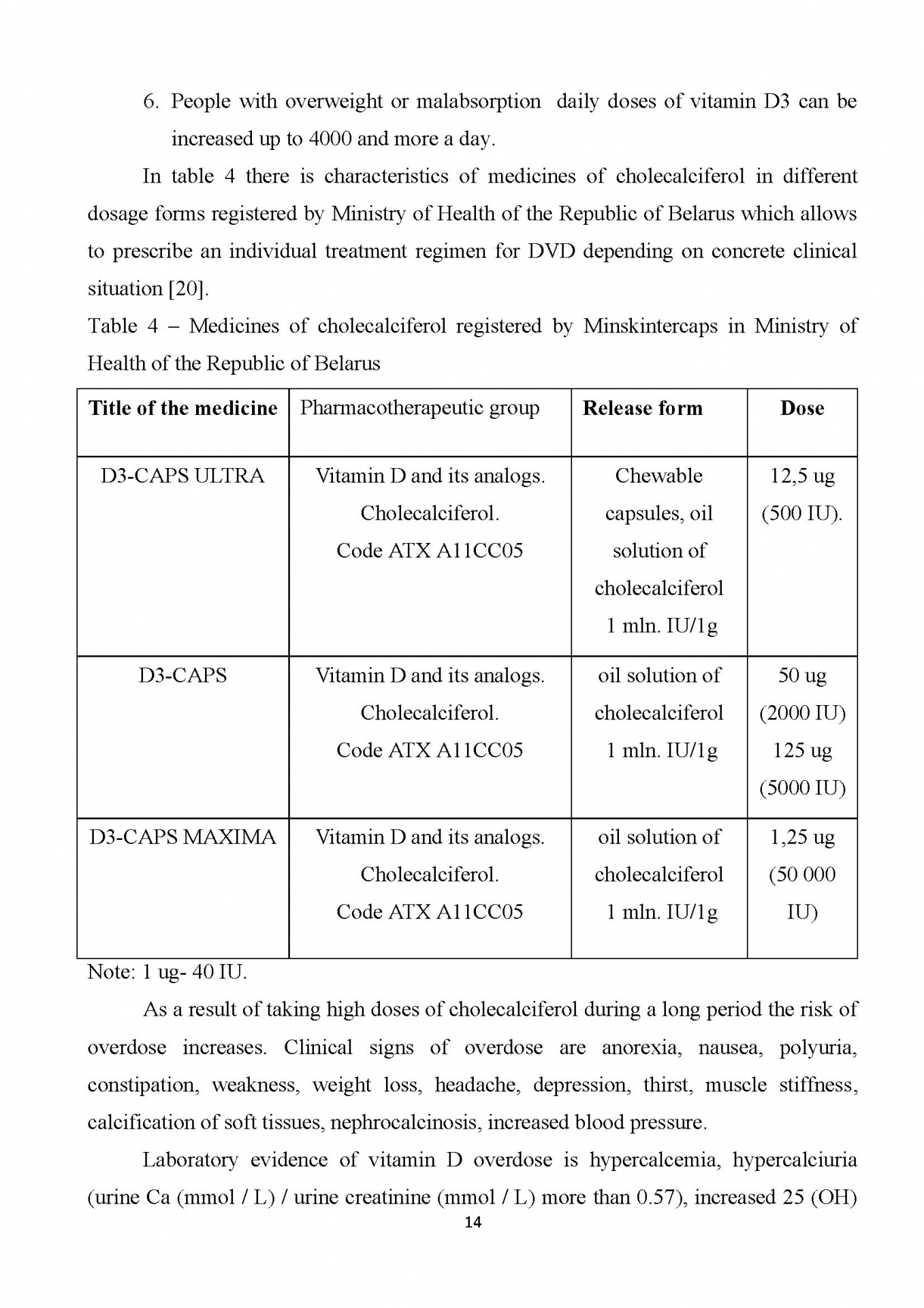
Note: 1 ug- 40 IU.
As a result of taking high doses of cholecalciferol during a long period the risk of overdose increases. Clinical signs of overdose are anorexia, nausea, polyuria, constipation, weakness, weight loss, headache, depression, thirst, muscle stiffness, calcification of soft tissues, nephrocalcinosis, increased blood pressure.
Laboratory evidence of vitamin D overdose is hypercalcemia, hypercalciuria (urine Ca (mmol / L) / urine creatinine (mmol / L) more than 0.57), increased 25 (OH) D level in more than 100 ng/ml. Hypercalcemic crisis developing with the increase of calcium level in blood till 4 mmol/L can be fatal as a result of depression of nervous activity and coma.
Vitamin D3 medicines are contraindicated in patients with hypercalcemia,
hypercalciuria, nephrolithiasis, tendency to allergic reactions to the components of the composition of the medicine. Due to the increased risk of hypercalcemia and hypercalciuria Vitamin D medicines are not prescribed for diagnosed granulomatosis,
sarcoidosis, bone metastases, Williams syndrome [5,9,2].
Conclusion. When prescribing calcium and vitamin D medicines
the attending physician must make every effort to achieve adequate adherence to treatment and get the best result in terms of primary and secondary prevention of HVD and complications connected with it. At the same time a regular laboratory monitoring of calcium-phosphorus metabolism indicators is necessary to exclude hypercalcemia especially when prescribing high doses of vitamin D. Monotherapy of DVD with cholecalciferol has been carried out for years and if there is no any effect or in case of concrete clinical situations especially with renal osteodystrophies active metabolites of calcitriol and alfacalcidol are prescribed. More details about biological effects of vitamin D you may find on website https://vitamindwiki.com.